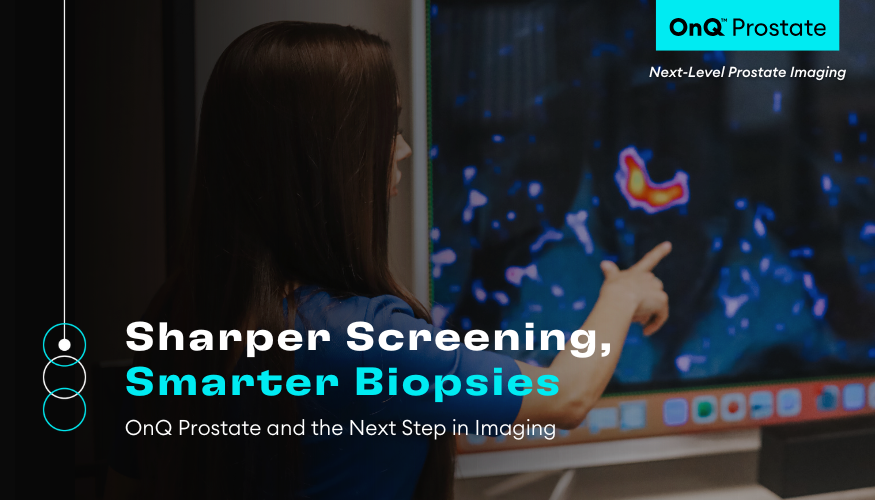
For many urologists, prostate MRI can feel a bit like a black box from which only the radiologist is able to interpret the images in any meaningful way. This may not be a problem if you have a subspecialty-trained expert reader on speed dial. But what happens if you don’t or if he or she happens to be sick that day? Most urologists in the real world have experienced some level of inter-reader variability which may have resulted in avoidable biopsies, missed diagnoses, and uncertainty with equivocal lesions. One option to help mitigate this variability is to use of the many prostate MRI AI tools on the market that have demonstrated expert-level detection accuracy. However, the truth is that whether the results come from a human radiologist or an AI model, this doesn’t help you – as the urologist – actually see the cancer better for yourself.
When urologists feel comfortable interacting with images themselves, many doors open in terms of the potential for providing more personalized patient care. The benefits of integrating imaging more deeply in your practice may range from improved selection of patients for biopsy, performing more intentional targeting biopsies (cognitive or software fusion), and even something as simple yet meaningful as improving patient communication. When patients have their clinician show and explain their imaging results to them, they feel a greater sense of trust in the clinical decision-making progress.
In the post-diagnostic setting, the urologist’s confidence in their own ability to utilize imaging may hold even more weight for the patient if they may be a candidate for active surveillance and focal therapy. In active surveillance, MRI has the potential to help tailor biopsy protocols to an individual’s risk of upgrading – helping avoid unnecessary biopsies and trigger critical ones. For focal therapy, it becomes absolutely essential that the MRI is used to help both qualify the appropriate patients and to plan the margins for treatment.
In all of the scenarios described above, standard prostate MRI is inherently limited and it may seem like the only way for a urologist to gain proficiency is to undergo intensive radiological training. But there is a better way that actually helps everyone involved in the patient’s care be more confident in accurately identifying and delineating potentially clinically significant prostate cancer on MRI – including less specialized or less experienced radiologists as well as urologists. OnQ Prostate takes prostate imaging to the next level using a patented technology call Restriction Spectrum Imaging (RSI), an advanced diffusion MRI technique that is specifically honed to the cellular characteristics of cancer. The color-coded images provided by OnQ Prostate – which display areas of highly restricted diffusion overlaid onto the anatomy – are quickly becoming a go-to for urologists looking to quickly and easily visualize findings and integrate them into their clinical decisions and procedure plans. With this added clarity, OnQ Prostate amplifies the value of prostate MRI at every step in the patient journey. The results are more reliable reads – with decreased inter-reader variability, more precise procedures – with enhanced targeting capabilities for biopsy and focal therapy, and overall more confident care – with bridged gaps between urologists, radiologists, and patients.