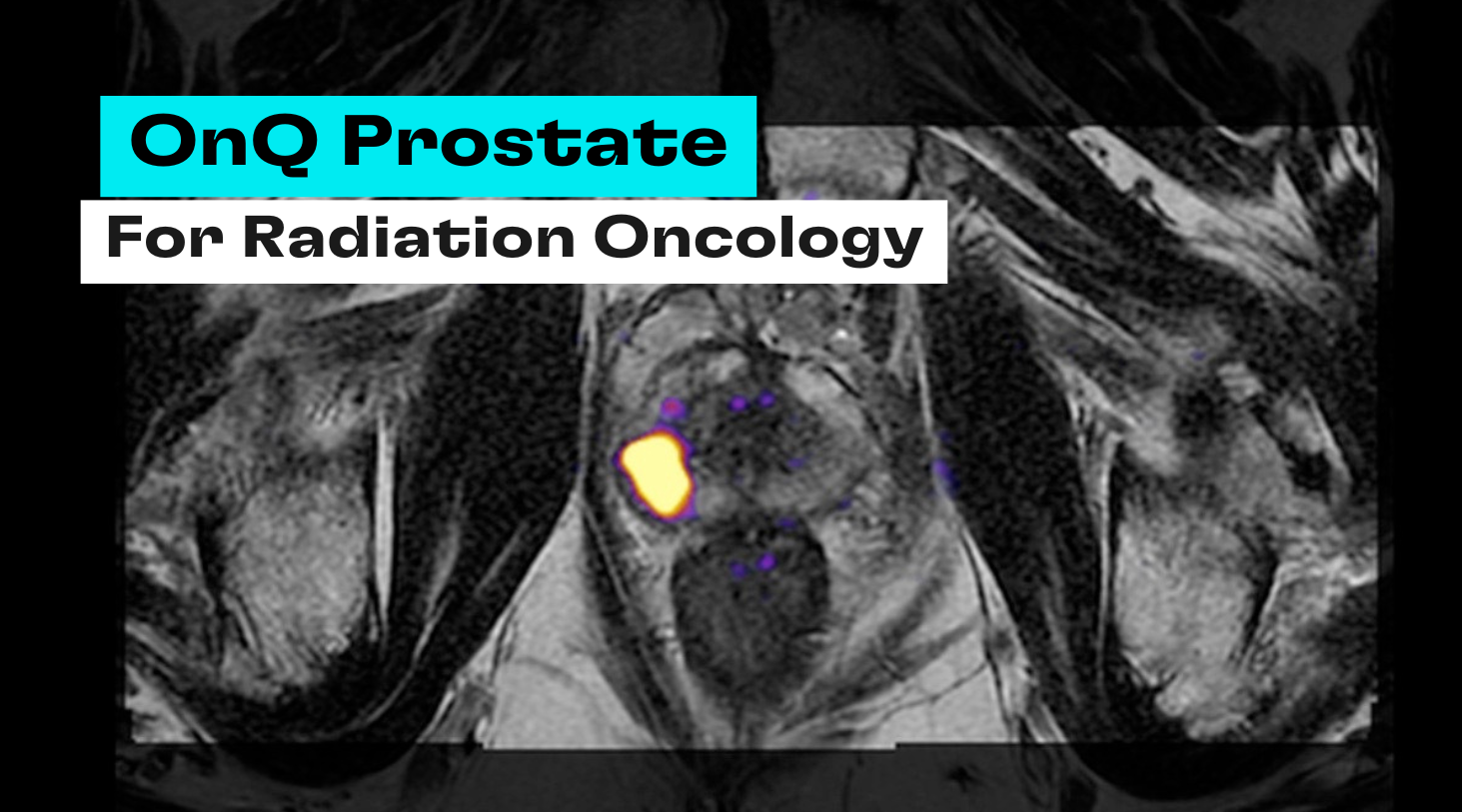
Radiation therapy as an option for men with prostate cancer has been greatly improved over recent years with technological advancements in the way radiation is delivered and with image guidance. Within radiation oncology, treatment options generally fall into two categories: External Beam Radiation Therapy (EBRT) and internal radiation also known as Brachytherapy. While it is said that Brachytherapy is the original focal therapy for prostate cancer, and OnQ Prostate is certainly relevant for that as well, this blog will mainly focus on EBRT.
A New Era of Precision with SBRT
Essentially all EBRT these days is Intensity-Modulated Radiation Therapy (IMRT) and Image-Guided Radiation Therapy (IGRT) – radiation oncologists love their acronyms! Even more modern and more precise is a technique called Stereotactic Body Radiation Therapy (SBRT), also known as SAbR (Stereotactic Ablative Radiotherapy), which allows high doses of radiation to be delivered over fewer sessions. Multiple randomized trials have supported SBRT as a safe and effective treatment including HYPO-RT and PACE-B.
Why Focal Boosting Matters & The MRI Barrier
So what does this have to do with OnQ Prostate? In 2021 the Journal of Clinical Oncology published results of the Focal Lesion Ablative Microboost in Prostate Cancer (FLAME) trial, which showed that the addition of a focal boost to the dominant intraprostatic lesion (DIL) visible on multi-parametric MRI resulted in improved biochemical disease-free survival (bDFS) for patients with localized intermediate- and high-risk prostate cancer without increasing toxicity or negatively impacting quality of life. These results seem almost too good to be true and show essentially no down-side to implementing focal boosting into clinical practice. The only catch is that the DIL must be able to be accurately delineated and contoured on the MRI and those in the FLAME trial were done by expert radiologists.
The researchers in the ReIGNITE Radiation Therapy Boost Trial (Lui et al. 2023) had two hypotheses: 1) radiation oncologists would struggle to accurately delineate tumors on convention MRI and 2) using Restriction Spectrum Imaging (RSI), the technology used in OnQ Prostate, would significantly improve their accuracy. Spoiler alert: they were right! Participants in the study, which included 44 radiation oncologists from 9 different nations, completely missed the expert-defined target in 13.6% of attempts on convention MRI versus 0.0% with RSI. Without RSI, the participants’ contoured volumes only covered a median 41% of the expert-defined target compared to 78% with RSI.
Ultimately, the ReIGNITE trial uncovered a significant barrier to adoption of the FLAME trial findings and delivering the benefits to real-world patients, which is the ability to accurately delineate and contour DILs on conventional MRI. More importantly, it offered a promising solution through RSI. OnQ Prostate is FDA-cleared and CE Mark-pending.
Cortechs.ai is excited to be at the forefront of advanced imaging to empower the delivery of true precision therapies that minimize harm to patients while maximizing oncologic outcomes and quality of life.