By Brandon Steach
Are medical Artificial Intelligence (AI) products reimbursed through health insurers? Should we apply the same fee for service model like prior medical devices before AI?
AI refers to the ability of computer systems to perform tasks that typically require human intelligence. AI systems are designed to analyze and learn from data, so it can make predictions or recommendations based on that data.
Between 2015 and 2020, the United States Food and Drug Administration (FDA) and the European Commission (EC) cleared 222 and 240 AI devices, respectively, for clinical use, often under the “software as a medical device” or similar designation (1). In August 2020, the US Centers for Medicare & Medicaid Services (CMS) announced its intention to provide coverage for the first AI-specific Common Procedural Terminology (CPT) code and the creation of the first New Technology Add-On Payment (NTAP) for an AI device (2). This CPT designation was given for a product IDX-DR (digital diagnostics), which is a deep learning algorithm to diagnose diabetic retinopathy from fundoscopic images in the outpatient setting. There are 7 other AI products that are reimbursable via the NTAP designation. NTAP designations only last for no more than 3 years for a specific indication. In summary, there are currently only 3.6% of the FDA cleared AI products that have a CMS approved reimbursement.
Not having a direct relationship to offset the costs on insurers (like previous medical devices) has limited clinical AI adoption.
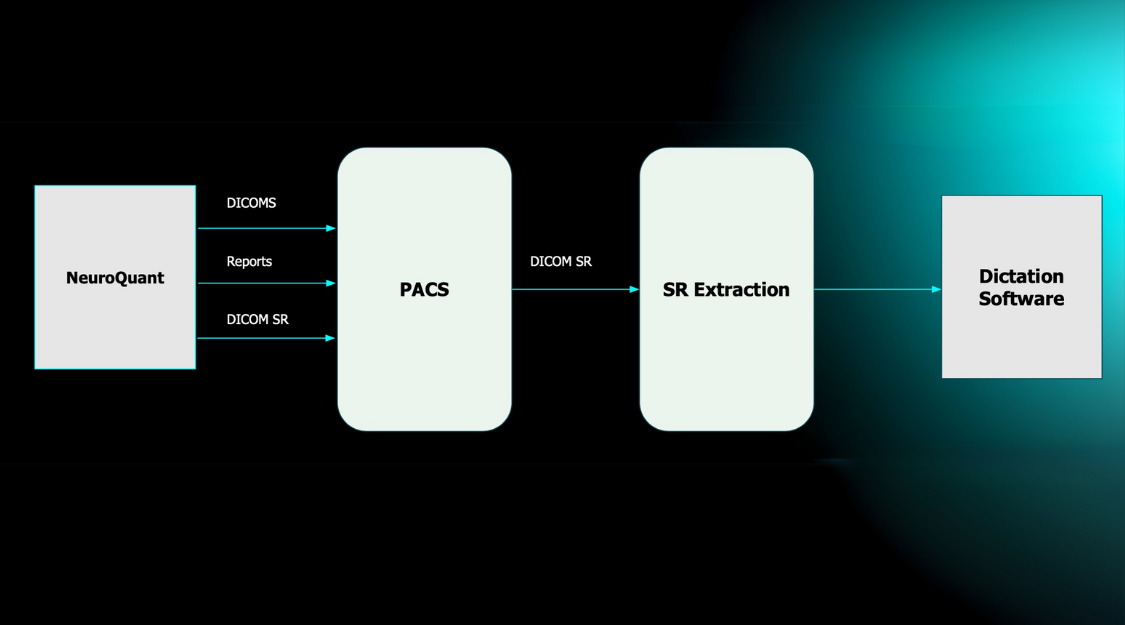
Quantitative MRI (QMRI) was not one of the technologies included in these initial approved reimbursable AI products, including our flagship product NeuroQuant. Historically, and currently, QMRI is loosely associated with supplementary CPT Codes 76376 & 763777 that are to be used in combination with a brain MRI. Although widely accepted as the preferred CPT billing code for AI post-processing, many insurance providers do not recognize this code, as it has been over-utilized and misrepresented over the years. Other conditions also apply to bills for utilizing these codes.
In order to charge for these codes, it is stated on page 370 of the CPT 2012 Professional Edition code book that “concurrent physician supervision is required for the reporting” of the three-dimensional (3D) codes 76376 and 76377 (3). Although it is not required to document physician involvement, it is advisable in case of an audit.
Per the AMA/ACR Clinical Examples in Radiology, concurrent physician supervision, as noted in the new 3D codes 76376 and 76377, defines a temporal relationship to creating the 3D volume rendered images. ‘Concurrent’ means active participation in and monitoring of the reconstruction process that includes: design of the anatomic region that is to be reconstructed, determination of the tissue types and actual structures to be displayed (eg, bone, organs, and vessels), determination of the images or cine loops that are to be archived, and monitoring and adjustment of the 3D work product.
Incorporating AI applications into the current fee for service model as described above has been quite challenging, as the rapid rate of development and adoption has outpaced CMS in evaluating if and where these types of applications fit into the FFS reimbursement model. To date, there is no formal guidance regarding standards for CMS coverage for AI (4).
One alternative to the current model is shifting towards value-based payment models. CMS has set goals to shift every Medicare beneficiary and a majority of Medicaid beneficiaries to a value-based care arrangement by 2030 (5). These efforts are already captured measures by the Healthcare Effectiveness Data and Information Set (HEDIS). The value of AI could then be captured by demonstrating how it had a reward, positive effect on quality metrics.
Another potential reimbursement model is the time-limited add-on reimbursement, like CMS’s transitional drug add-on payment (TDAP), which helps cover new pharmaceuticals that aren’t bundled or episode-based payments. Also, payers could consider providing financial incentives for AI devices that demonstrate interoperability and applicability across multiple health settings that can perform on a diverse patient group in premarket testing.
In conclusion, AI has a reimbursement problem and trying to conform AI to prior medical device reimbursement methodology has stifled commercialization and limited access to the majority of the population.
References:
- Muehlematter, U. J., Daniore, P. & Vokinger, K. N. Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015–20): a comparative analysis. Lancet Digit. Health 3, e195–e203 (2021).
- Chen, M. M., Golding, L. P. & Nicola, G. N. Who will pay for AI? Radio. Artif. Intell. 3, e210030 (2021).
- American College of Radiology. ACR Radiology Coding Source for March-April 2012 Q and A. https://www.acr.org/Advocacy-and-Economics/Coding-Source/ACR-Radiology-Coding-Source-for-March-April-2012-Q-and-A (2012)
- Parikh, R.B., Helmchen, L.A. Paying for artificial intelligence in medicine. npj Digit. Med. 5, 63 (2022). https://doi.org/10.1038/s41746-022-00609-6
- Centers for Medicare & Medicaid Services. Medicare coverage of innovative technologies (MCIT). https://www.cms.gov/blog/medicare-coverage-innovative technologies-mcit (2021).