Louis Gagnon, Diviya Gupta, George Mastorakos, Nathan White, Vanessa Goodwill, Carrie McDonald, Thomas Beaumont, Christopher Conlin, Tyler Seibert, Jona Hattangandi-Gluth, Santosh Kesari, Jessica Schulte, David Piccioni, Anders Dale, Niky Farid, Jeffrey Rudie
Abstract
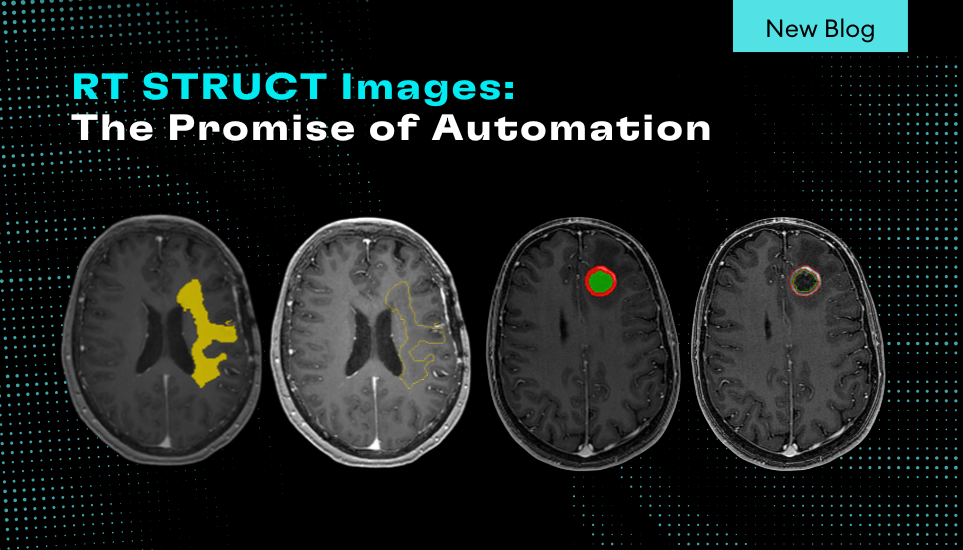
Multimodal MRI is used for the evaluation of tumor burden in glioblastoma (GBM) patients after surgical resection, radiation, and chemotherapy. However, it can be challenging to identify non-enhancing infiltrative tumor and differentiate recurrent enhancing tumor from post-treatment changes. Restriction spectrum imaging (RSI), an advanced multishell diffusion technique, has shown promise in distinguishing cellular tumor from edema and enhancing post-treatment changes including pseudoprogression and radiation necrosis. We developed a convolutional network (nnUNet) that incorporates traditional multimodal MRI with DSC perfusion and RSI to detect and quantify enhancing and nonenhancing cellular tumor in post-treatment glioblastoma patients. This cellular tumor segmentation network was evaluated in a cohort of 186 post-treatment GBM patients (55.5 +/- 13.7 years, 158 male) with 243 timepoints using 5-fold cross validation. Cellular tumor volumes were then used to predict overall survival (OS) and progression free survival (PFS) in 94 patients with imaging within 3 months of initial surgery. Accuracy for segmenting cellular tumor as measured by the Dice-similarity coefficient was 0.77 (IQR 0.55-0.87) and the AUC of the ROC curve for detecting residual/recurrent tumor compared to post-treatment changes was 0.86. The predicted cellular tumor volumes were an independent hazard over age, sex, GTR status and conventional enhancing residual tumor for both OS (p=0.0003) and PFS (p=0.0004). The tumor segmentation network was validated in an external dataset of 22 GBM patients (55 timepoints) with a median Dice of 0.73 and AUC of 0.91. Survival prediction was validated in a different external dataset of 70 post-treatment GBM patients, with cellular tumor volumes being an independent predictor of OS (p=0.03). In conclusion, deep learning models incorporating advanced imaging can accurately segment enhancing and nonenhancing cellular tumor, which can help distinguish recurrent/residual tumor from post-treatment changes and predict OS and PFS.